كشف الشركاء الخفيين: التحري عن العدوى الميكروبية التآزرية لالتهابات المسالك البولية بين كبار السن
DOI:
https://doi.org/10.32007/jfacmedbaghdad2416الكلمات المفتاحية:
الميكروبات المشتركة, اصابات المسالك البولية, المرضى كبار السنالملخص
الخلفية: تحتل العدوى الميكروبية المشتركة جزءا كبيرا من التهابات المسالك البولية وخاصة عند كبار السن. ومثل هذه الإصابات تكون مخفية، وذلك لغلبة نوع واحد على النوع الآخر.
الأهداف: هدفت هذه الدراسة إلى الكشف عن مسببات العدوى المشتركة باستخدام تقنيات الزرع والجزيئي.
المرضى وطرق العمل: تم جمع مائة عينة ادرار سريرية من مرضى كبار السن يعانون من التهابات المسالك البولية، وتراوحت أعمار المرضى بين (55-75) سنة ونسبة الذكور والإناث هي (1:1). تم زرع هذه العينات على اوساط زرعية انتقائية وتفريقية. تم تنقية وتشخيص البكتريا المعزولة باستخدام نظام فايتيك. تم إجراء اختبار الحساسية للمضادات الحيوية لتقييم نمط المقاومة لمضادات الحياة. تم استخلاص الحمض النووي البكتيري وتم تصميم بادئات محددة لهذه الدراسة لتضخيم جينات المقاومة armA وrmtG بتقنية PCR.
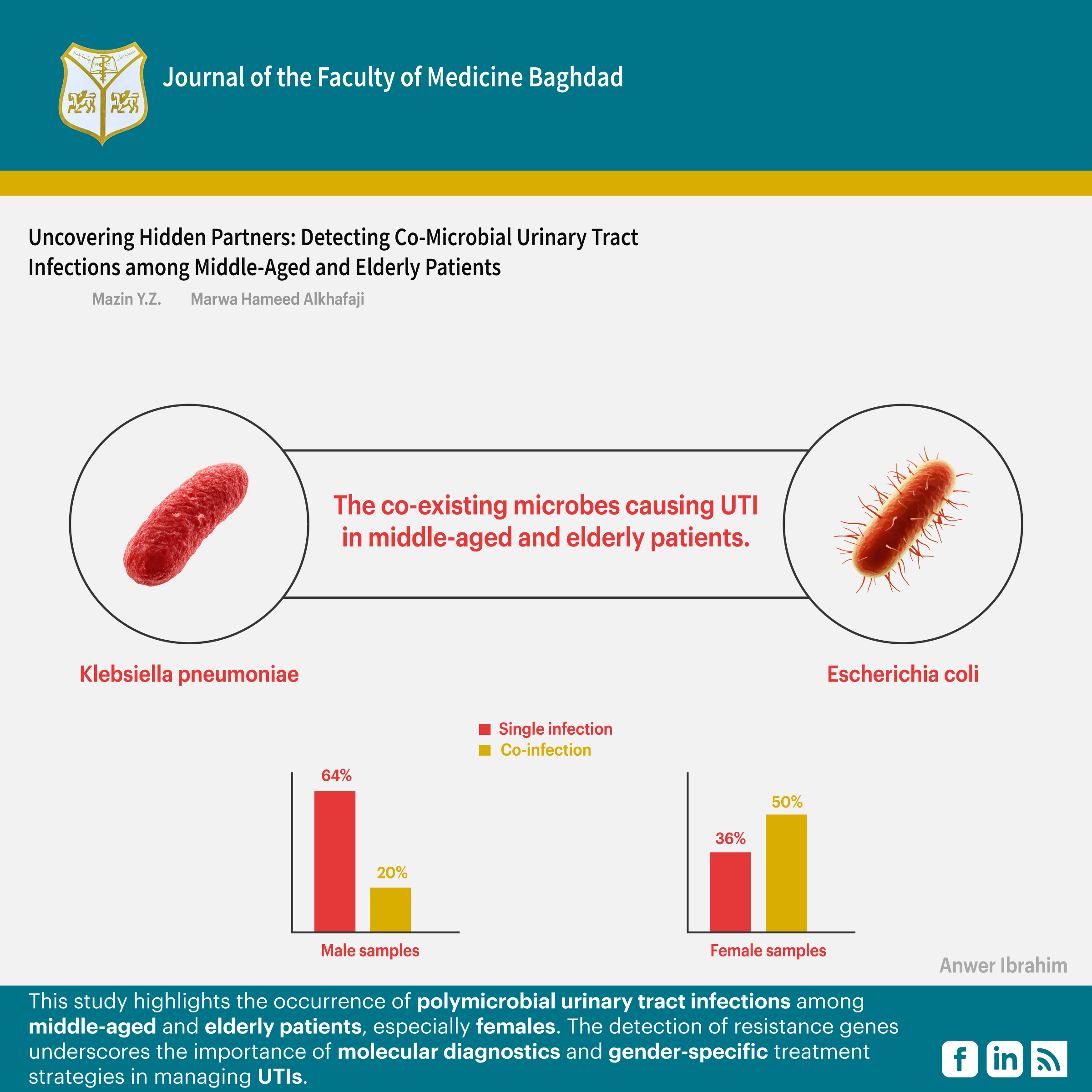
النتائج: كانت الكليبسيلا الرئوية والإشريكية القولونية هي الميكروبات المشتركة السائدة التي تسبب التهاب المسالك البولية في المرضى المسنين. وكانت هذه الميكروبات المشتركة مقاومة للمضادات الحيوية aminoglycoside. يحمل كلا من K. pneumoniae و E. coliجين armA بينما كان جين rmtG هو السائد في K.pneumoniae فقط.
الاستنتاج: هناك فروق ذات دلالة إحصائية بين الجنسين في معدلات الإصابة المشتركة، وخاصة بين الإناث الذين تتراوح أعمارهم بين 55-60 و55-69 سنة. حددت اختبارات الحساسية للمضادات الحيوية والتحليل الجيني جينات المقاومة armA وrmtG هي السائدة في عزلات (E. coliوK.pneumoniae) ولكن تم تحديد وجود rmtG في K.pneumoniaeفقط. تؤكد الدراسة على الحاجة إلى استراتيجيات علاج خاصة بجنس المريض والمراقبة المستمرة لمقاومة المضادات الحيوية في عدوى المسالك البولية.
المراجع
1. Rodriguez-Mañas L. Urinary tract infections in the elderly: a review of disease characteristics and current treatment options. Drugs in context. 2020 Jul 8;9. https://doi.org/10.7573/dic.2020-4-13.
2. Khalil MI, Alnoomani MN, Grasso III M. Asymptomatic Bacteriuria: A Contemporary Review. Current Bladder Dysfunction Reports. 2023 Mar; 18(1):29-35. https://doi.org/10.1007/s11884-022-00675-2.
3. Voidazan S, Albu S, Toth R, Grigorescu B, Rachita A, Moldovan I. Healthcare associated infections—a new pathology in medical practice?. International journal of environmental research and public health. 2020 Feb;17(3):760. https://doi.org/10.3390/ijerph17030760.
4. Rowe TA, Juthani-Mehta M. Urinary tract infection in older adults. Aging Health. 2013;9(5):519–528. https://doi.org/10.2217/ahe.13.38.
5. Goebel MC, Trautner BW, Grigoryan L. The five Ds of outpatient antibiotic stewardship for urinary tract infections. Clinical microbiology reviews. 2021 Dec 15; 34(4):e00003-20. https://doi.org/10.1128/CMR.00003-20.
6. Wagenlehner FM, Bjerklund Johansen TE, Cai T, Koves B, Kranz J, Pilatz A, et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nature Reviews Urology. 2020 Oct; 17(10):586-600. https://doi.org/10.1038/s41585-020-0362-4.
7. Medina-Polo J, Naber KG, Johansen TE. Healthcare-associated urinary tract infections in urology. GMS infectious diseases. 2021. https://doi.org/10.3205/id000074.
8. Turyatunga G, Wito SG, Muwagunzi E. Antibacterial Susceptibility Patterns of Common Bacterial Species Associated with Urinary Tract Infections in Patients Attending Kam Medical and Diagnostic Centre, Kampala Uganda. SJHR Africa. 2021 Jun 13; 2(6):10. https://doi.org/10.51168/sjhrafrica.v2i6.32.
9. Jacobsen SM, Stickler DJ, Mobley HL, Shirtliff ME. Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. CMR. 2008 Jan;21(1):26-59. https://doi.org/10.1128/CMR.00019-07.
10. Flatby HM, Ravi A, Liyanarachi KV, Afset JE, Rasheed H, Brumpton BM, et al. A genome-wide association study of susceptibility to upper urinary tract infections. JID. 2024 Dec 15;230(6):e1334-43. https://doi.org/10.1093/infdis/jiae231.
11. Zagaglia C, Ammendolia MG, Maurizi L, Nicoletti M, Longhi C. Urinary tract infections caused by uropathogenic Escherichia coli strains—new strategies for an old pathogen. Microorganisms. 2022 Jul 14; 10(7):1425. https://doi.org/10.3390/microorganisms10071425.
12. Henly EL, Norris K, Rawson K, Zoulias N, Jaques L, Chirila PG, et al. Impact of long-term quorum sensing inhibition on uropathogenic Escherichia coli. JAC. 2021 Apr 1; 76(4):909-19. https://doi.org/10.1093/jac/dkaa517.
13. Sora VM, Meroni G, Martino PA, Soggiu A, Bonizzi L, Zecconi A. Extraintestinal pathogenic Escherichia coli: virulence factors and antibiotic resistance. Pathogens. 2021 Oct 20; 10(11):1355. https://doi.org/10.3390/pathogens10111355.
14. AL-Jubouri SS, Shami AM. Molecular Detection of Cephalosporin Resistance Genes in Escherichia coli Isolated from Urinary Tract Infections in Baghdad Hospitals. IJB. 2022;21(2):145-52. https://www.jige.uobaghdad.edu.iq/index.php/IJB/article/view/489.
15. Tomulescu C, Moscovici M, Lupescu I, Stoica Rm, Vamanu A. A Review: Klebsiella pneumoniae, Klebsiella Oxytoca. Rom. Biotechnol. Lett. 2021; 26:2567-86. https://doi.org/10.25083/rbl/26.3/2567.2586.
16. Al-Abeadi RS, Suhail AA, Almousawi AE. Retraction: An overview of Klebsiella pneumoniae: History, taxonomy, epidemiology, pathogenicity, virulence factors and treatment. InAIP Conference Proceedings 2023 Dec 22 (Vol. 2977, No. 1, p. 040062). AIP Publishing LLC. https://doi.org/10.1063/5.0182174.
17. Jabarah MA. Cephalosporins are the not the cause of death in a pregnant with urinary tract infection; A case Report: Cephalosporins and treatment of urinary tract infection during pregnancy. J Fac Med Baghdad. 2022 Apr 24;64(1):42-6. https://doi.org/10.32007/jfacmedbagdad.6411881.
18. Yang, W. and Hu, F., 2022. Research updates of plasmid-mediated aminoglycoside resistance 16S rRNA methyltransferase. Antibiotics, 11(7), p.906.. https://doi.org/10.3390/antibiotics11070906.
19. Neut C. Carriage of multidrug-resistant bacteria in healthy people: Recognition of several risk groups. Antibiotics. 2021 Sep 25; 10(10):1163. https://doi.org/10.3390/antibiotics10101163
20. Munson E, Carroll KC. Summary of novel bacterial isolates derived from human clinical specimens and nomenclature revisions published in 2018 and 2019. JCM. 2021 Jan 21; 59(2):10-128. https://doi.org/10.1128/jcm.01309-20.
21. Kohlerschmidt DJ, Mingle LA, Dumas NB, Nattanmai G. Identification of aerobic Gram-negative bacteria. In: Green LH, Goldman E. Practical handbook of microbiology 2021 May 4 (pp. 59-70). https://doi.org/10.1201/9781003099277-7.
22. Sadeq ZE, Lafta IJ. Tigecycline is the Most Effective against Multi-Drug Resistant Klebsiella pneumoniae Recovered from Burn Wound Infections in Two Hospitals in Al-Kut City, Iraq. Iraqi J Sci. 2024 Feb 29:659-74. https://doi.org/10.24996/ijs.2024.65.2.7.
23. Sinawe H, Casadesus D. Urine culture. Study Guide from StatPearls Publishing, Treasure Island (FL), 01 May 2023. https://europepmc.org/article/nbk/nbk557569.
24. Tzelepi E, Giakkoupi P, Sofianou D, Loukova V, Kemeroglou A, Tsakris A. Detection of extended-spectrum β-lactamases in clinical isolates of Enterobacter cloacae and Enterobacter aerogenes. Journal of clinical microbiology. 2000 Feb 1; 38(2):542-6. https://doi.org/10.1128/JCM.38.2.542-546.2000.
25. Maniatis T. Molecular cloning. A laboratory manual. 1982. https://cir.nii.ac.jp/crid/1574231874811406208.
26. Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. European Association of Urology guidelines on sexual and reproductive health—2021 update: male sexual dysfunction. European urology. 2021 Sep 1; 80(3):333-57. https://doi.org/10.1016/j.eururo.2021.06.007.
27. Coppola N, Cordeiro NF, Trenchi G, Esposito F, Fuga B, Fuentes-Castillo D, et al. Imported one-day-old chicks as trojan horses for multidrug-resistant priority pathogens harboring mcr-9, rmtG, and extended-spectrum β-lactamase genes. Applied and Environmental Microbiology. 2022 Jan 25;88(2):e01675-21. https://doi.org/10.1128/AEM.01675-21.
28. Delgado-Blas JF, Valenzuela Agüi C, Marin Rodriguez E, Serna C, Montero N, Saba CK, Gonzalez-Zorn B. Dissemination routes of carbapenem and pan-aminoglycoside resistance mechanisms in hospital and urban wastewater canalizations of Ghana. Msystems. 2022 Feb 22; 7(1):e01019-21. https://doi.org/10.1128/msystems.01019-21.
29. Wilfinger WW, Mackey K, Chomczynski P. Effect of pH and ionic strength on the spectrophotometric assessment of nucleic acid purity. Biotechniques. 1997 Mar 1; 22(3):474-81. https://doi.org/10.2144/
30. Harding C, Mossop H, Homer T, Chadwick T, King W, Carnell S, et al. Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women: multicentre, open label, randomised, non-inferiority trial. bmj. 2022 Mar 9; 376. https://doi.org/10.1136/bmj-2021-0068229.
31. ALzubaidi SJ, Alkhafaji MH. Molecular Detection of bla TEM and bla CTX-M Genes in Clinical and Food-Borne Klebsiella pneumoniae isolates. J Med. Chem. Sci. 2023; 6 (7): 1706-1713 https://doi.org/10.26655/JMCHEMSCI.2023.7.20.
32. Devi P, Khan A, Chattopadhyay P, Mehta P, Sahni S, Sharma S, et al. Co-infections as modulators of disease outcome: minor players or major players?. Frontiers in microbiology. 2021 Jul 6;12:664386. https://doi.org/10.3389/fmicb.2021.664386.
33. Bail L, Ito CA, Arend LN, Pilonetto M, da Silva Nogueira K, Tuon FF. Distribution of genes encoding 16S rRNA methyltransferase in plazomicin-nonsusceptible carbapenemase-producing Enterobacterales in Brazil. Diagnostic Microbiology and Infectious Disease. 2021 Feb 1; 99(2):115239. https://doi.org/10.1016/j.diagmicrobio.2020.115239.
34. Martins ER, Bueno MF, Francisco GR, Casella T, de Oliveira Garcia D, Cerdeira LT, et al. Genome and plasmid context of two rmtG-carrying Enterobacter hormaechei isolated from urinary tract infections in Brazil. Journal of global antimicrobial resistance. 2020 Mar 1; 20:36-40. https://doi.org/10.1016/j.jgar.2019.06.020.
35. Devanga Ragupathi NK, Veeraraghavan B, Muthuirulandi Sethuvel DP, Anandan S, Vasudevan K, Neeravi AR, Daniel JL, et al. First Indian report on genome-wide comparison of multidrug-resistant Escherichia coli from blood stream infections. PLoS One. 2020 Feb 26; 15(2):e0220428. https://doi.org/10.1371/journal.pone.0220428.
36. Zhang X, Li Q, Lin H, Zhou W, Qian C, Sun Z, et al. High-level aminoglycoside resistance in human clinical Klebsiella pneumoniae complex isolates and characteristics of armA-carrying IncHI5 plasmids. Frontiers in Microbiology. 2021 Apr 7; 12:636396. https://doi.org/10.3389/fmicb.2021.636396.
37. Caméléna F, Morel F, Merimèche M, Decousser JW, Jacquier H, Clermont O, et al. Genomic characterization of 16S rRNA methyltransferase-producing Escherichia coli isolates from the Parisian area, France. JAC. 2020 Jul 1; 75(7):1726-35. https://doi.org/10.1093/jac/dkaa105.
38. Cox G, Stogios PJ, Savchenko A, Wright GD. Structural and molecular basis for resistance to aminoglycoside antibiotics by the adenylyltransferase ANT (2 ″)-Ia. MBio. 2015 27; 6(1):10-128. https://doi.org/10.1128/mBio.02180-14,
39. Ramirez MS, Tolmasky ME. Amikacin: uses, resistance, and prospects for inhibition. Molecules. 2017 19; 22(12):2267. https://doi.org/10.3390/molecules22122267.
40. Wang N, Luo J, Deng F, Huang Y, Zhou H. Antibiotic combination therapy: A strategy to overcome bacterial resistance to aminoglycoside antibiotics. Front. Pharm. 2022 Feb 23; 13:839808. https://doi.org/10.3389/fphar.2022.839808.
41. AL TT. Molecular Identification of Klebsiella pneumoniae Isolated from UTI Patients in Al-Anbar Governorate and Study Its Antibiotic Resistance and determination of Antimicrobial Activity of Flax seed Oil. IJB. 2022;21 (2):612-622. https://jige.uobaghdad.edu.iq/index.php/IJB/article/view/537











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..