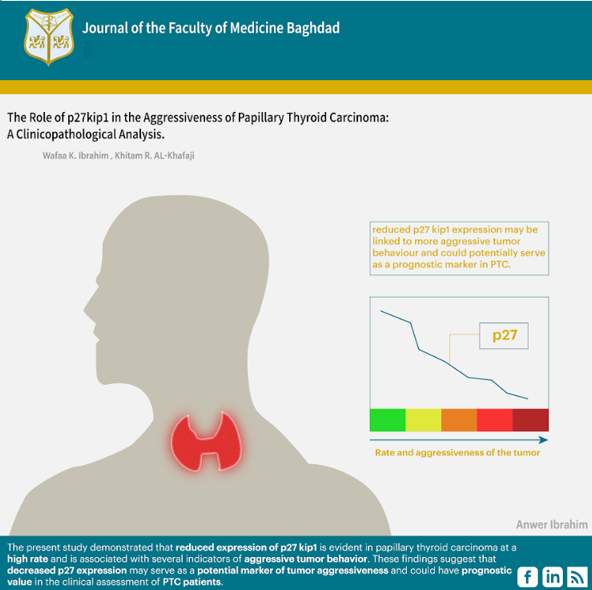
The Role of p27kip1 in the Aggressiveness of Papillary Thyroid Carcinoma: A Clinicopathological Analysis
DOI:
https://doi.org/10.32007/jfacmedbaghdad3147Keywords:
Clinicopathological parameters, Cyclin-dependent kinase inhibitor p27kip1, Immunohistochemistry, Papillary thyroid carcinoma, Tumor aggressivenessAbstract
Background: Cell-cycle-regulating proteins, including cyclin-dependent kinase inhibitor 1B p27kip1, have been researched in different malignancies, including thyroid carcinoma, and their association with tumor aggressiveness and recurrence has been examined in many tumors.
Objective: This research aimed to examine the clinicopathological relevance of reduced cyclin-dependent kinase inhibitor 1B p27kip1 expression in papillary thyroid carcinoma and its association with the clinicopathological parameters indicative of papillary thyroid carcinoma aggressiveness.
Methods: Formalin-fixed, paraffin-embedded tissue blocks were obtained from histologically confirmed cases of papillary thyroid carcinoma diagnosed between June 2022 and June 2023 at the National Center for Teaching Laboratories, Medical City Complex, Baghdad, Iraq. A total of 60 papillary thyroid carcinoma samples were included in the study. Immunohistochemical analysis was performed to assess the expression of the p27 protein. The study further evaluated the association between cyclin-dependent kinase inhibitor 1B p27kip1 expression and various clinicopathological parameters, including patients’ age, sex, papillary thyroid carcinoma subtypes, tumor size, capsular invasion, multifocality, extrathyroidal extension, and lymph node metastasis.
Results: A decrease in the expression of cyclin-dependent kinase inhibitor 1B p27kip1 of less than 10% was observed in 37 out of 60 cases (61.7%). The correlation with clinicopathological parameters revealed a significant decrease in expression of cyclin-dependent kinase inhibitor 1B p27kip1 associated with female sex, classical variant PTC, infiltrative tumors, large tumor size (2-2.5 cm), and multifocal lesions.
Conclusion: Reduced expression of cyclin-dependent kinase inhibitor 1B p27kip1; (<10%) was observed at a relatively high rate in papillary thyroid carcinoma. A significant correlation was found between decreased cyclin-dependent kinase inhibitor 1B p27kip1 expression and several clinicopathological features, including infiltrative pattern tumors, large tumor size, and multifocality. These findings suggest that reduced cyclin-dependent kinase inhibitor 1B p27kip1 expression may be linked to more aggressive tumor behaviour and could potentially serve as a prognostic marker in PTC.
Received: May 2025
Revised: Aug. 2025
Accepted: Aug. 2025
Published Online: Sept. 2025
References
1. Li D, Li J, Zhou J, Xiao Q, Gao H. Metastatic papillary thyroid carcinoma with no primary tumor in the thyroid gland: a case report and review of literature. TCR. 2022;11(1):299. https://doi.org/10.21037/tcr-21-1780. DOI: https://doi.org/10.21037/tcr-21-1780
2. Shank JB, Are C, Wenos CD. Thyroid cancer: global burden and trends. Indian Journal of Surgical Oncology. 2022:1-6.
https://doi.org/10.1007/s13193-021-01429-y . DOI: https://doi.org/10.1007/s13193-021-01429-y
3. Weller S, Chu C, Lam AK-y. Assessing the Rise in Papillary Thyroid Cancer Incidence: A 38-Year Australian Study Investigating WHO Classification Influence. Journal of Epidemiology and Global Health. 2025;15(1):9. https://doi.org/10.1007/s44197-025-00354-5. DOI: https://doi.org/10.1007/s44197-025-00354-5
4. Carnazza M, Quaranto D, DeSouza N, Moscatello AL, Garber D, Hemmerdinger S, et al.. The Current Understanding of the Molecular Pathogenesis of Papillary Thyroid Cancer. International Journal of Molecular Sciences. 2025;26(10):4646. https://doi.org/10.3390/ijms26104646. DOI: https://doi.org/10.3390/ijms26104646
5. Kaliszewski K, Diakowska D, Miciak M, Jurkiewicz K, Kisiel M, Makles S, et al.. The Incidence Trend and Management of Thyroid Cancer-What Has Changed in the Past Years: Own Experience and Literature Review. Cancers. 2023;15(20):4941. https://doi.org/10.3390/cancers15204941. DOI: https://doi.org/10.3390/cancers15204941
6. Gao MZ, Omer TM, Miller KM, Simpson MC, Bukatko AR, Gedion K, et al.. Thyroid Cancer Incidence and Trends in United States and Canadian Pediatric, Adolescent, and Young Adults. Cancers. 2025;17(9):1429. https://doi.org/10.3390/cancers17091429. DOI: https://doi.org/10.3390/cancers17091429
7. Furqan S, Ahmed A, Batool S, Islam N. Outcome analysis of differentiated thyroid cancer: Experience from tertiary care in Karachi. PJMS. 2024;40(11):2631. https://doi.org/10.12669/pjms.40.11.7036. DOI: https://doi.org/10.12669/pjms.40.11.7036
8. Jabbar MQA, Mutlak NS, Hussein WA, Sulaiman TI. Incidental thyroid carcinoma. JFac Med Baghdad. 2016;58(3):245-9. https://doi.org/10.32007/jfacmedbagdad.583258. DOI: https://doi.org/10.32007/jfacmedbagdad.583258
9. Sulaiman TI, Sarsam MK. the The Role of Ultrasound in the Diagnosis of Malignant Thyroid Nodules. J Fac Med Baghdad. 2020;62(3). https://doi.org/10.32007/jfacmedbagdad.6231772. DOI: https://doi.org/10.32007/jfacmedbagdad.6231772
10. Mahoney FS. Investigating The Cooccurrence Of Papillary Thyroid Carcinoma Among Patients With Oncocytic Pathology: Is There Evidence Of Causation? 2025.
11. Özcan B, Cin M, Demirbaş ZE. Can Aggressive Papillary Thyroid Carcinoma Variants With Oncocytıc Morphology (Tall Cell and Hobnail Variants) be Detected Cytologically? Is the Differentiation as Straightforward as Reported? Cytopathology. 2025. https://doi.org/10.1111/cyt.13502. DOI: https://doi.org/10.1111/cyt.13502
12. Ghossein R, Katabi N, Dogan S, Shaha AR, Tuttle RM, Fagin JA, et al.. Papillary thyroid carcinoma tall cell subtype (PTC‐TC) and high‐grade differentiated thyroid carcinoma tall cell phenotype (HGDTC‐TC) have different clinical behaviour: a retrospective study of 1456 patients. Histopathology. 2024;84(7):1130-8. https://doi.org/10.1111/his.15157. DOI: https://doi.org/10.1111/his.15157
13. Yoshino R, Ujiie N, Yasuda S, Kitada M. Multiple Lung Metastases of Papillary Thyroid Carcinoma Detected by Detailed Pathological Examination: A Case Series. Cureus. 2025;17(3). https://doi.org/10.7759/cureus.80112. DOI: https://doi.org/10.7759/cureus.80112
14. Zhang J, Xu S. High aggressiveness of papillary thyroid cancer: from clinical evidence to regulatory cellular networks. Cell Death Discovery. 2024;10(1):378. https://doi.org/10.1038/s41420-024-02157-2. DOI: https://doi.org/10.1038/s41420-024-02157-2
15. Sorrenti S, Carbotta G, Di Matteo FM, Catania A, Pironi D, Tartaglia F, et al.. Evaluation of clinicopathological and molecular parameters on disease recurrence of papillary thyroid cancer patient: A retrospective observational study. Cancers. 2020;12(12):3637. https://doi.org/10.3390/cancers12123637. DOI: https://doi.org/10.3390/cancers12123637
16. Zhao S, Zhang Z, Zhang X, Wu X, Chen Y, Min X, et al.. Sonographic characteristics and clinical characteristics combined with nomogram for predicting the aggressiveness of papillary thyroid carcinoma coexisted with Hashimoto's thyroiditis. Brazilian Journal of Otorhinolaryngology. 2024;90(5):101456. https://doi.org/10.1016/j.bjorl.2024.101456. DOI: https://doi.org/10.1016/j.bjorl.2024.101456
17. Kim M, Cho SW, Park YJ, Ahn HY, Kim HS, Suh YJ, et al.. Clinicopathological characteristics and recurrence-free survival of rare variants of papillary thyroid carcinomas in Korea: a retrospective study. Endocrinology and metabolism. 2021;36(3):619-27. https://doi.org/10.3803/EnM.2021.974 DOI: https://doi.org/10.3803/EnM.2021.974
18. McCovins J-m. Characterization of the Cell Cycle Dependent Kinase Inhibitor p27KIP1 in the Stem-Like Properties of Breast Cancer Stem Cells: Texas Southern University; 2022.
19. Fhu CW, Ali A. Dysregulation of the ubiquitin proteasome system in human malignancies: a window for therapeutic intervention. Cancers. 2021;13(7):1513. https://doi.org/10.3390/cancers13071513 . DOI: https://doi.org/10.3390/cancers13071513
20. Tyrna P, Procyk G, Szeleszczuk Ł, Młynarczuk-Biały I. Different Strategies to Overcome Resistance to Proteasome Inhibitors-A Summary 20 Years after Their Introduction. IJMS. 2024;25(16):8949. https://doi.org/10.3390/ijms25168949 DOI: https://doi.org/10.3390/ijms25168949
21. Hussain AM, Lafta RK. Cancer trends in Iraq 2000-2016. Oman medical journal. 2021;36(1):e219.
https://doi.org/10.5001/omj.2021.18 . DOI: https://doi.org/10.5001/omj.2021.18
22. BY R, Salih DHH, division MFCD, / ocrCbiI, MOH, Hasan MAH, et al.. annual report of Iraq cancer registry 2020. 2020..
23. Niciporuka R, Nazarovs J, Ozolins A, Narbuts Z, Miklasevics E, Gardovskis J. Can we predict differentiated thyroid cancer behavior? role of genetic and molecular markers. Medicina. 2021;57(10):1131. https://doi.org/10.3390/medicina57101131 DOI: https://doi.org/10.3390/medicina57101131
24. Fu J, Liu J, Wang Z, Qian L. Predictive Values of Clinical Features and Multimodal Ultrasound for Central Lymph Node Metastases in Papillary Thyroid Carcinoma. Diagnostics. 2024;14(16):1770. https://doi.org/10.3390/diagnostics14161770 DOI: https://doi.org/10.3390/diagnostics14161770
25. Erickson LA, Yousef OM, Jin L, Lohse CM, Pankratz VS, Lloyd RV. p27kip1 expression distinguishes papillary hyperplasia in Graves' disease from papillary thyroid carcinoma. Modern Pathology. 2000;13(9):1014-9. https://doi.org/10.1038/modpathol.3880182
26. Iqneibi S, Nazzal J, Owda B, Sultan H, Amoudi R, Amarin JZ, et al.. Immunohistochemical Expression of p27Kip1, p57Kip2, Cyclin D1, Nestin, and Ki-67 in Ependymoma. Brain Sciences. 2022;12(2):282. https://doi.org/10.3390/brainsci12020282 DOI: https://doi.org/10.3390/brainsci12020282
27. Razavipour SF, Harikumar KB, Slingerland JM. p27 as a transcriptional regulator: new roles in development and cancer. Cancer research. 2020;80(17):3451-8. https://doi.org/10.1158/0008-5472.CAN-19-3663 DOI: https://doi.org/10.1158/0008-5472.CAN-19-3663
28. Hume S, Dianov GL, Ramadan K. A unified model for the G1/S cell cycle transition. Nucleic acids research. 2020;48(22):12483-501. https://doi.org/10.1093/nar/gkaa1002 DOI: https://doi.org/10.1093/nar/gkaa1002
29. Do S-I, Kim DH, Yang J-H, Pyo J-S, Kim K, Lee H, et al.. Decreased expression of p27 is associated with malignant transformation and extrathyroidal extension in papillary thyroid carcinoma. Tumor Biology. 2016;37:3359-64. https://doi.org/10.1007/s13277-015-4163-y DOI: https://doi.org/10.1007/s13277-015-4163-y
30. Hernandez-Prera JC, Riddle N, Gonzalez RS, Asa SL. Endocrine and Neuroendocrine Tumors: Updates From the 5th Edition of the World Health Organization "Blue Book". Archives of Pathology & Laboratory Medicine. 2025. https://doi.org/10.5858/arpa.2024-0315-RA DOI: https://doi.org/10.5858/arpa.2024-0315-RA
31. Sgambato A, Cittadini A, Faraglia B, Weinstein IB. Multiple functions of p27Kip1 and its alterations in tumor cells: a review. Journal of cellular physiology. 2000;183(1):18-27. https://doi.org/10.1002/(SICI)1097-4652(200004)183:1<18::AID-JCP3>3.0.CO;2-S DOI: https://doi.org/10.1002/(SICI)1097-4652(200004)183:1<18::AID-JCP3>3.0.CO;2-S
32. Guerra A, Marotta V, Deandrea M, Motta M, Limone PP, Caleo A, et al.. BRAF V600E associates with cytoplasmatic localization of p27kip1 and higher cytokeratin 19 expression in papillary thyroid carcinoma. Endocrine. 2013;44:165-71. https://doi.org/10.1007/s12020-012-9843-4 DOI: https://doi.org/10.1007/s12020-012-9843-4
33. Erickson LA, Yousef OM, Jin L, Lohse CM, Pankratz VS, Lloyd RV. p27kip1 expression distinguishes papillary hyperplasia in Graves' disease from papillary thyroid carcinoma. Modern Pathology. 2000;13(9):1014-9. https://doi.org/10.1038/modpathol.3880182 DOI: https://doi.org/10.1038/modpathol.3880182
34. Özbek B, Şensu S, AKYAY Z, GÜRBÜZ Y. Papiller Tiroid Karsinomunun Hematojen Yayılım Potansiyelini Öngörmek Mümkün mü?: P27 ile İmmünohistokimyasal Çalışma. Kocaeli Tıp Dergisi. 2024;13(1). https://doi.org/10.5505/ktd.2024.26042. DOI: https://doi.org/10.5505/ktd.2024.26042
35. Kim NY, Kim JH, Pyo J-S, Cho WJ. Clinicopathological significance of loss of p27kip1 expression in papillary thyroid carcinoma. The International Journal of Biological Markers. 2017;32(2):255-9. https://doi.org/10.5301/jbm.5000239. DOI: https://doi.org/10.5301/jbm.5000239
36. Pešutić-Pisac V, Punda A, Glunčić I, Bedeković V, Pranić-Kragić A, Kunac N. Cyclin D1 and p27 expression as prognostic factor in papillary carcinoma of thyroid: association with clinicopathological parameters. Croatian medical journal. 2008;49(5):643-9. https://doi.org/10.3325/cmj.2008.5.643. DOI: https://doi.org/10.3325/cmj.2008.5.643
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Wafaa K. Ibrahim, khitam R. Al-khafaji

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..