Radiological Patterns of Bronchogenic Carcinoma in a Sample of Iraqi Patients
DOI:
https://doi.org/10.32007/jfacmedbaghdad2432Keywords:
Bronchogenic carcinoma, Chest imaging, Computed Tomography, Iraqi patients, Radiological PatternsAbstract
Background: Bronchogenic carcinoma is considered one of the most common malignant diseases that affects both sexes. The radiological profile of bronchogenic cancer can prove to be of great assistance in the management of this disease.
Objectives: The current study aimed to assess a radiological profile for bronchogenic carcinoma in a sample of Iraqi patients.
Methods: A cross-sectional study that comprised a total of 100 patients affected with bronchogenic cancer in Al-Imamain Al-Kadhimain Medical City, Baghdad, Iraq, from the 1st of January to 31st of July 2020. Clinical characteristics, diagnostic modalities, the site of the tumor within the lung, radiological findings, and the histopathologic type of cancer, were recorded.
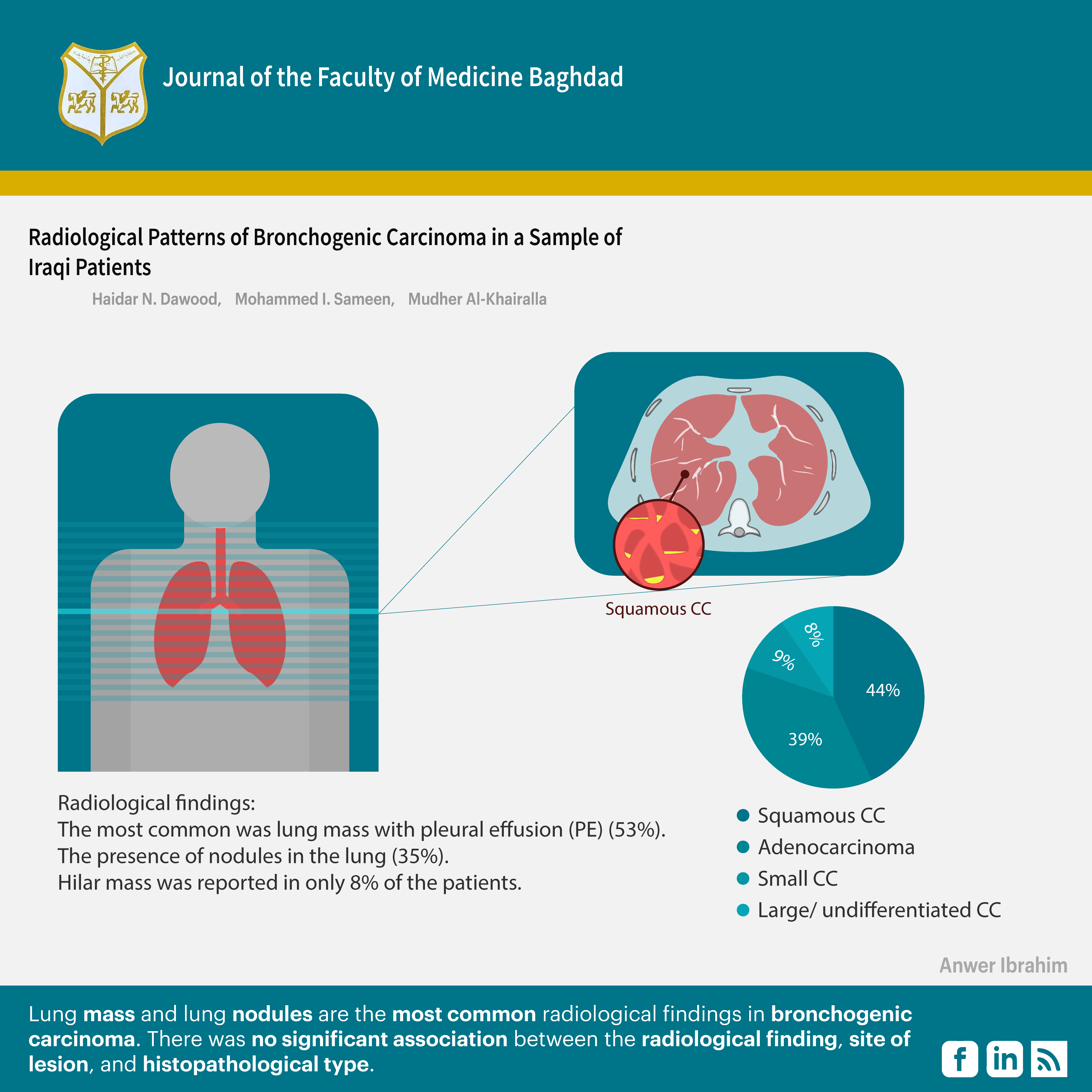
Results: The subjects consisted of 100 patients affected with bronchogenic carcinoma, 70% were males and 30% were females, and the mean age was 62.26±10.8 years. Also, 59% were ex\current smokers. The site of the tumour, according to the CT scan, was 44% in the left lung, 40% in the right lung, and 16% bilaterally. The most common histopathological type was squamous cell carcinoma, accounting for 44% of patients; the second type was adenocarcinoma (39%). The radiological findings showed 53% of the cases, the cancer was seen as a mass on imaging, while in 35% a solitary nodule was found
Conclusions: Lung mass and lung nodules are the most common radiological findings in bronchogenic carcinoma. There was no significant association between the radiological finding, site of lesion, and histopathological type.
References
1. Chao L, Shaoyuan L, Li D, Yan X, Xiaonan W, Hui W, et al. Global burden and trends of lung cancer incidence and mortality. Chin Med J (Engl). 2023 Mar 28;136(13):1583–1590. https://doi.org/10.1097/CM9.0000000000002529. DOI: https://doi.org/10.1097/CM9.0000000000002529
2. Cao W, Chen HD, Yu YW, Li N, Chen WQ. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Chin Med J 2021; 7:783–791. https://doi.org/10.1097/CM9.0000000000001474. DOI: https://doi.org/10.1097/CM9.0000000000001474
3. Howlader N, Noone AM, Krapcho M, et al: SEER Cancer Statistics Review, 1975-2017. Bethesda, MD, National Cancer Institute, 2020. https://seer.cancer.gov/csr/1975_2017/.
4. Agonsanou H, Figueiredo R, Bergeron M. Risk factors for the development of lung cancer around the world: a review. Explor Med. 2023; 4:1168–88. https://doi.org/10.37349/emed.2023.00201. DOI: https://doi.org/10.37349/emed.2023.00201
5. Cagnur E. Lung Cancer Risk factors - A Review Article. EJMA 2022;2(4):159–162 https://doi.org/10.14744/ejma.2022.36036. DOI: https://doi.org/10.14744/ejma.2022.36036
6. Mohan A, Garg A, Gupta A, Satyaranjan S, Chandrashekhar Ch, Vishal V, et al. Clinical profile of lung cancer in North India: a 10-year analysis of 1862 patients from a tertiary care center. Lung India 2020;37(03):190-197.
https://doi.org/10.4103/lungindia.lungindia_333_19.
7. Haastrup PF, Jarbøl DE, Balasubramaniam K, Sætre LM, Søndergaard J, Rasmussen S. Predictive values of lung cancer alarm symptoms in the general population: a nationwide cohort study. NPJ Primary Care Respiratory Medicine. 2020 Apr 7;30(1):15. https://doi.org/10.1038/s41533-020-0173-3. DOI: https://doi.org/10.1038/s41533-020-0173-3
8. Ganti AKP, Loo BWJ, Bassetti M, Collin B, Anne Ch, Thomas A, et al. Small cell lung cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(12):1441-1464. https://doi.org/10.6004/jnccn.2021.0058. DOI: https://doi.org/10.6004/jnccn.2021.0058
9. Ettinger DS, Wood DE, Aisner DL, Wallace A, Jessica R, Ankit B, et al. Non-small cell lung cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20(05):497-530. https://doi.org/10.6004/jnccn.2022.0025 DOI: https://doi.org/10.6004/jnccn.2022.0025
10. Foley RW, Nassour V, Oliver HC, Toby H, Vidan M, Graham R, et al. Chest x-ray in suspected lung cancer is harmful. Eur Radiol. 2021;31(8):6269-6274. https://doi.org/10.1007/s00330-021-07708-0. DOI: https://doi.org/10.1007/s00330-021-07708-0
11. Dwyer-Hemmings L, Fairhead C. The diagnostic performance of chest radiographs for lung malignancy in symptomatic primary-care populations: a systematic review and meta-analysis. BJR Open. 2021;3(1): 20210005. https://doi.org/10.1259/bjro.20210005 DOI: https://doi.org/10.1259/bjro.20210005
12. Purandare NC, Rangarajan V. Imaging of lung cancer: Implications on staging and management. Indian J Radiol Imaging. 2015;25(2):109-120. https://doi.org/10.1080/09553002.2018.1511930 .
13. Purandare NC, Rangarajan V. Imaging of lung cancer: Implications on staging and management. Indian J Radiol Imaging. 2015;25(2):109-120. https://doi.org/10.4103/0971-3026.155831. DOI: https://doi.org/10.4103/0971-3026.155831
14. Anant M, Avneet G, Aditi G, Satyaranjan S, Chandrashekhar Ch, Vishal V, et al. Clinical profile of lung cancer in North India: A 10-year analysis of 1862 patients from a tertiary care centre. Lung India. 2020 May-Jun; 37(3): 190-197. https://doi.org/10.4103/lungindia.lungindia_333_19. DOI: https://doi.org/10.4103/lungindia.lungindia_333_19
15. Senthil K, Jayakumar N, Janani S, Madhankumar V, Kaviyarasi P. Clinical, Pathological and Radiological Profile of Lung Carcinoma in A Tertiary Care Centre of South India. Int J Acad Med Pharm 2024; 6 (1); 858-862. https://doi.org/10.47009/jamp.2024.6.1.168.
16. Alberto R, Mariano P, Virginia C, Enric C, Teresa M, Delvys R, et al. Lung cancer symptoms at diagnosis: results of a nationwide registry study. ESMO 2020;5:e001021. https://doi.org/10.1136/esmoopen-2020-001021 DOI: https://doi.org/10.1136/esmoopen-2020-001021
17. Girija S, Jacek M, Shanta R. Gender Differences in Smoking Among U.S. Working Adults. Am J Prev Med. 2014 Jul 18;47(4):467–475. https://doi.org/10.1016/j.amepre.2014.06.013 DOI: https://doi.org/10.1016/j.amepre.2014.06.013
18. Shiels MS, Graubard BI, McNeel TS, Kahle L, Freedman ND. Trends in smoking-attributable and smoking-unrelated lung cancer death rates in the United States, 1991-2018. JNCI. 2024 May 1;116(5):711-6. https://doi.org/10.1093/jnci/djad256 DOI: https://doi.org/10.1093/jnci/djad256
19. Mohammed M, Sabah N, Okba F, Fahmi H Bnar J, Soran H, et al. Resectability in bronchogenic carcinoma: A single center experience. Oncol Lett. 2023 Apr 12;25(6):219. https://doi.org/10.3892/ol.2023.13805 DOI: https://doi.org/10.3892/ol.2023.13805
20. Chandramouli M, Giridhar B. Clinicopathological Profile of Patients with Lung Carcinoma in a Tertiary Care Center. J Health Allied Sci NU:2021; 11:18-20. https://doi.org/10.1055/s-0040-1718977 DOI: https://doi.org/10.1055/s-0040-1718977
21. Singh N, Aggarwal AN, Gupta D, Behera D, Jindal SK. Unchanging clinico-epidemiological profile of lung cancer in north India over three decades. Cancer Epidemiol 2010; 34:101-4. https://doi.org/10.1016/j.canep.2009.12.015 DOI: https://doi.org/10.1016/j.canep.2009.12.015
22. Prasad R, James P, Kesarwani V, Gupta R, Pant MC, Chaturvedi A, et al. Clinicopathological study of bronchogenic carcinoma. Respirology 2004; 9:557-60. https://doi.org/10.1111/j.1440-1843.2004.00600.x DOI: https://doi.org/10.1111/j.1440-1843.2004.00600.x
23. Akhil K, Vanita N, Vijay P, Nandini M, Amit J, Amit K, et al. Clinical Profile, Practice Pattern, and Outcomes with First-Line Therapy in ALK-Positive Lung Cancer: Real-World Data From Resource-Constrained Settings. Clinical and Research Reports. 2023; 4(1). https://doi.org/10.1016/j.jtocrr.2022.100443 DOI: https://doi.org/10.1016/j.jtocrr.2022.100443
24. Yanting Z, Salvatore V, Eileen M, Mengmeng L, Jaione E, Eric Ch, et al. Global variations in lung cancer incidence by histological subtype in 2020: a population-based study. Lancet Oncol. 2023 Nov;24(11):1206-1218. https://doi.org/10.1016/S1470-2045(23)00444-8 DOI: https://doi.org/10.1016/S1470-2045(23)00444-8
25. Prabha R, Davis NT, Muhammed AK, Fernandez SS. A study on clinical, radiological, and cytologic features of lung cancer. AJMS. 2023 Oct 2;14(10):276-80. https://doi.org/10.3126/ajms.v14i10.53086 DOI: https://doi.org/10.3126/ajms.v14i10.53086
26. Rohit R, Chetan B. Study of clinical profile of lung cancer cases at a tertiary care center. MedPulse International JOMed. September 2019; 11(3): 227-230. https://doi.org/10.26611/102111318 DOI: https://doi.org/10.26611/102111318
27. Gharraf HS, Mehana SM, ElNagar MA. Role of CT in differentiation between subtypes of lung cancer; is it possible?. Egypt J Bronchol. 2020;14:28. https://doi.org/10.1186/s43168-020-00027-w DOI: https://doi.org/10.1186/s43168-020-00027-w
28. Chakrabortty R, Siddiqua DR, Paul SK, Rahman S, Biswas SK. Histopathological Patterns of Lung Cancer along with Clinico-Radiological Correlation in a Tertiary Care Hospital in Bangladesh. JOMed. 2022 Jul 1; 23(2). https://doi.org/10.3329/jom.v23i2.60629 DOI: https://doi.org/10.3329/jom.v23i2.60629
29. Watanabe Y, Kusumoto M, Yoshida A, Kenji S, Hisao A, Koji T. Surgically Resected Solitary Cavitary Lung Adenocarcinoma: AIN right lung association Between Clinical, Pathologic, and Radiologic Findings and Prognosis. Ann Thorac Surg. 2015; 99:968-74. https://doi.org/10.1016/j.athoracsur.2014.10.040 DOI: https://doi.org/10.1016/j.athoracsur.2014.10.040
30. Bo J, Qiwen Z, Xinmeng Q, Jun Z, Meina W, Tongtong A. Survival comparison of right and left side non‐small cell lung cancer in stage I–IIIA patients: A Surveillance Epidemiology and End Results (SEER) analysis. Thorac Cancer. 2019 Jan 9;10(3):459–471. https://doi.org/10.1111/1759-7714.12959.
31. Adnan M, Kassim M. Sultan, Muhammed W, Firas R. Bronchogenic carcinoma in sample of Iraqi patients, Fiber optic bronchoscope findings. J Fac Med Baghdad. 2014: 56(4): 367 – 371. https://doi.org/10.32007/jfacmedbagdad.564547. DOI: https://doi.org/10.32007/jfacmedbagdad.564547
32. Jia B, Zheng Q, Qi X, Zhao J, Wu M, An T, Wang Y, Zhuo M, Li J, Zhao X, Yang X. Survival comparison of right and left side non‐small cell lung cancer in stage I–IIIA patients: A Surveillance Epidemiology and End Results (SEER) analysis. Thoracic cancer. 2019 Mar;10(3):459-71. https://doi.org/10.1111/1759-7714.12959. DOI: https://doi.org/10.1111/1759-7714.12959
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Haider N. Dawood, Mohammed I. Sameen, Mudher Al-Khairalla

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..