Maternal Serum Tumor Necrosis Factor Level in Women with Hyperemesis Gravidarum
DOI:
https://doi.org/10.32007/jfacmedbaghdad3137Keywords:
Assessment; , hyperemesis; , tumor necrosis factor-α; , womenAbstract
Background: Between 0.3% and 2% of pregnant women experience hyperemesis gravidarum. It is recognized by persistent and unexplained vomiting and dehydration, and the diagnosis is confirmed by significant loss of weight, usually more than 5% of the pre-pregnancy weight. Tumor necrosis factor-α is a multipotent cytokine that affects a vast array of cells. It is now well accepted that the tumor necrosis factor-α is crucial in the very early stages of pregnancy.
Objectives: To assess the relationship between the tumor necrosis factor-α and hyperemesis gravidarum.
Methods: This case-control study was carried out at the Baghdad Teaching Hospital, Obstetrics and Gynecology Department, from 1 January to 1 November 2022. The study involved 50 pregnant women, who suffered from hyperemesis gravidarum (mild or severe) as the case group, and another 50 healthy pregnant women as the control group, in the first trimester. The (Pregnancy-Unique Quantification of Emesis and Nausea) Index was used to evaluate the severity of the symptoms. Five milliliters of venous blood were taken to measure the tumor necrosis factor-α.
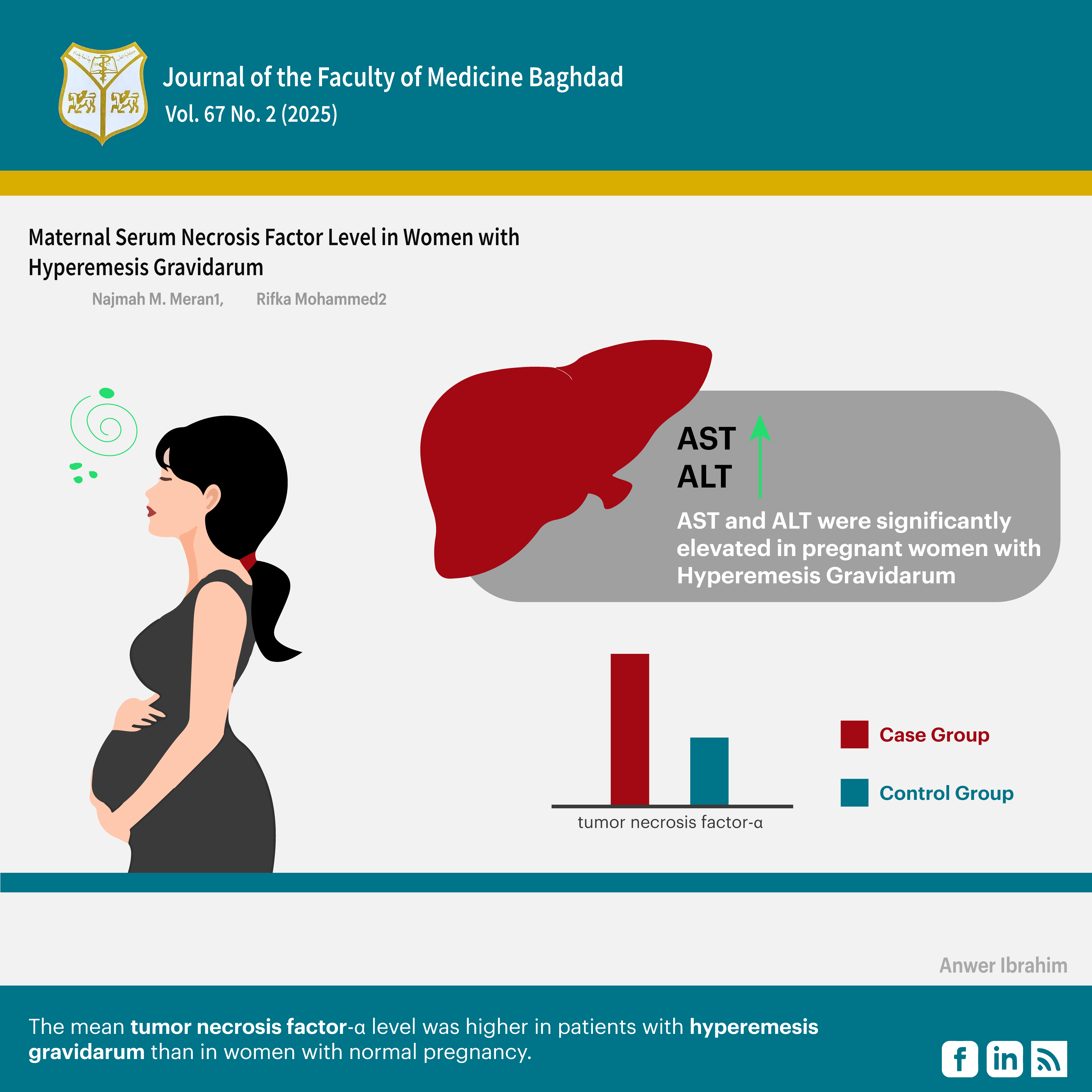
Results: In contrast to the women in the control group, pregnant women with hyperemesis gravidarum had a mean hemoglobin that was significantly lower (10.8) g/dL compared to the control group (11.5) g/dL and their liver enzymes were significantly higher except for alkaline phosphatase, (294.4) IU/L compared to the control group (49.5) IU/L. Their mean tumor necrosis factor-α level was also significantly higher, (200.6) pg/ml versus (96.34) pg/ml in the control group.
Conclusion: The mean tumor necrosis factor-α level was higher in patients with hyperemesis gravidarum than in women with normal pregnancy.
Received: March 2025
Revised: May 2025
Accepted: June 2025
Published Online: June 2025
Published: July 2025
References
Austin K, Wilson K, Saha S. Hyperemesis gravidarum. Nutrition in Clinical Practice. 2019; 34(2):226-41. https://pubmed.ncbi.nlm.nih.gov/30334272/ DOI: https://doi.org/10.1002/ncp.10205
2. Cunningham F, Leveno K, Bloom S, Spong CY, Dashe J. Williams obstetrics: Mcgraw-hill; 2018, 25th edition. dokumen.pub_williams-obstetrics-25th-edition-25nbsped-1259644332-9781259644337 (1).pdf
3. Dypvik J, Pereira AL, Tanbo TG, Eskild A. Maternal human chorionic gonadotrophin concentrations in very early pregnancy and risk of hyperemesis gravidarum: A retrospective cohort study of 4372 pregnancies after in vitro fertilization. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2018; 221:12-6. https://pubmed.ncbi.nlm.nih.gov/29227846/ DOI: https://doi.org/10.1016/j.ejogrb.2017.12.015
4. Puri M, Punetha D, Maan M and Burute S. Transient hyperthyroidism in hyperemesis gravidarum. International Journal of Clinical Obstetrics and Gynaecology, 2019, 3(1), 131-135. https://doi.org/10.33545/gynae.2019.v3.i1c.22 DOI: https://doi.org/10.33545/gynae.2019.v3.i1c.22
5. Nelson-Piercy C, Dean C, Shehmar M, Gadsby R, O'Hara M, Hodson K, et al. The Management of Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum, BJOG, 2024;131:e1-e30. https://doi.org/10.1111/1471-0528.17739 DOI: https://doi.org/10.1111/1471-0528.17739
6. Hada A, Minatani M, Wakamatsu M, Koren G, Kitamura T. The Pregnancy Unique Quantification of Emesis and Nausea (PUQE-24): Configural, Measurement, and Structural Invariance between Nulliparas and Multiparas and across Two Measurement Time Points. Healthcare. 2021; 9(11):1553. https://pubmed.ncbi.nlm.nih.gov/34828598/ DOI: https://doi.org/10.3390/healthcare9111553
7. You K, Gu H, Yuan Z, Xu X. Tumor Necrosis Factor Alpha Signaling and Organogenesis. Front. Cell Dev. Biol., 30 July 2021,Volume 9 :1-9 https://doi.org/10.3389/fcell.2021.727075 DOI: https://doi.org/10.3389/fcell.2021.727075
8. Azizieh FY, Raghupathy RG. Tumor necrosis factor-α and pregnancy complications: a prospective study. Med Princ Pract. 2015; 24(2):165-70. https://pubmed.ncbi.nlm.nih.gov/25501617/ DOI: https://doi.org/10.1159/000369363
9. Liu C, Zhao G, Qiao D, Wang L, He Y, Zhao M, et al. Emerging Progress in Nausea and Vomiting of Pregnancy and Hyperemesis Gravidarum: Challenges and Opportunities. Frontiers in Medicine,2022,(8):1-17. https://doi.org/10.3389/fmed.2021.809270 DOI: https://doi.org/10.3389/fmed.2021.809270
10. Nurmi M, Rautava P, Gissler M, Vahlberg T, Polo-Kantola P. Readmissions due to hyperemesis gravidarum: a nationwide Finnish register study. Archives of Gynecology and Obstetrics. 2022:1-11. https://link.springer.com/article/10.1007/s00404-022-06448-w DOI: https://doi.org/10.1007/s00404-022-06448-w
11. Alimah U, Dona S, Hestiyana N, editors. Relationship of age and parity of mother with the event of hyperemesis gravidarum: Literature review. International Conference on Health and Science; 2021. https://ocs.unism.ac.id/index.php/ICoHS/article/view/572
12. Thakur M, Gautam J, Dangal G. Severity of Hyperemesis Gravidarum and Associated Maternal factors. J Nepal Health Res Counc [Internet]. 2019; 17(3): 293-296. Available from: https://doi.org/10.33314/jnhrc.v17i3.2113. DOI: https://doi.org/10.33314/jnhrc.v17i3.2113
13. Türkmen H. The effect of hyperemesis gravidarum on prenatal adaptation and quality of life: a prospective case–control study. Journal of Psychosomatic Obstetrics & Gynecology. 2020; 41(4):282-9. https://pubmed.ncbi.nlm.nih.gov/31651204/ DOI: https://doi.org/10.1080/0167482X.2019.1678020
14. Febrianti R. The Relationship of Hyperemesis Gravidarum with Anemia in First Trimester Pregnant Women at the Midwife Clinic Yani Delitua in 2022. International Archives of Medical Sciences and Public Health. 2022; 3(2):7-13. https://www.pcijournal.org/index.php/iamsph/article/view/391
15. Salah E, Soliman M. The correlation between helicobacter pylori Infection, hyperemesis gravidarum, and anemia among pregnant females. Effect of treatment. 2017; 7(3) :100-104. https://ebwhj.journals.ekb.eg/article_5062_9b594a2f2991201f03cede0b4286e940.pdf DOI: https://doi.org/10.21608/ebwhj.2017.5062
16. Michihata N, Shigemi D, Sasabuchi Y, Matsui H, Jo T, Yasunaga H. Safety and effectiveness of Japanese herbal Kampo medicines for the treatment of hyperemesis gravidarum. International Journal of Gynecology & Obstetrics. 2019; 145(2):182-6. https://pubmed.ncbi.nlm.nih.gov/30734286/ DOI: https://doi.org/10.1002/ijgo.12781
17. Gaba N, Gaba S. Study of liver dysfunction in hyperemesis gravidarum. Cureus. 2020; 12(6). https://pubmed.ncbi.nlm.nih.gov/32699704/ DOI: https://doi.org/10.7759/cureus.8709
18. Sasamori Y, Tanaka A, Ayabe T. Liver disease in pregnancy. Hepatology Research. 2020; 50(9):1015-23. https://onlinelibrary.wiley.com/doi/abs/10.1111/hepr.13540 DOI: https://doi.org/10.1111/hepr.13540
19. Guarino M, Cossiga V, Morisco F. The interpretation of liver function tests in pregnancy. Best Practice & Research Clinical Gastroenterology. 2020; 44- 45:101667. https://pubmed.ncbi.nlm.nih.gov/32359686/ DOI: https://doi.org/10.1016/j.bpg.2020.101667
20. Florentin M, Parthymos I, Agouridis AP, Liamis G. Hyperemesis gravidarum: a benign condition of pregnancy or a challenging metabolic disorder? European Journal of Case Reports in Internal Medicine. 2020; 7(12). https://www.ejcrim.com/index.php/EJCRIM/article/download/1979/2400?inline=1 DOI: https://doi.org/10.12890/2020_001979
21. Weiss N, Mochel F, Rudler M, Demeret S, Lebray P, Conti F, et al. Peak hyperammonemia and atypical acute liver failure: The eruption of a urea cycle disorder during hyperemesis gravidarum. Journal of Hepatology. 2018; 68(1):185- 92. https://www.sciencedirect.com/science/article/abs/pii/S0168827817322894 DOI: https://doi.org/10.1016/j.jhep.2017.09.009
22. Popa SL, Barsan M, Caziuc A, Pop C, Muresan L, Popa LC, et al. Life-threatening complications of hyperemesis gravidarum. Exp Ther Med. 2021; 21(6):1-13. https://www.spandidos-publications.com/10.3892/etm.2021.10074 DOI: https://doi.org/10.3892/etm.2021.10074
23. Fejzo MS, Trovik J, Grooten IJ, Sridharan K, Roseboom TJ, Vikanes Å, et al. Nausea and vomiting of pregnancy and hyperemesis gravidarum. Nature reviews Disease primers. 2019; 5(1):1-17. https://pubmed.ncbi.nlm.nih.gov/31515515/ DOI: https://doi.org/10.1038/s41572-019-0110-3
24. Fedorka CE, Ali HE-S, Scoggin KE, Loux SC, Ball BA, Troedsson MH. Tumor necrosis factor signaling during equine placental infection leads to pro-apoptotic and necroptotic outcomes. Journal of Reproductive Immunology. 2022; 152:103655. https://pubmed.ncbi.nlm.nih.gov/35716439/ DOI: https://doi.org/10.1016/j.jri.2022.103655
25. Özgökçe Ç, Öcal A, Ermiş IS. Expression of NF-κB and VEGF in normal placenta and placenta previa patients. Advances in clinical and experimental medicine: official organ Wroclaw Medical University. 2022. https://pubmed.ncbi.nlm.nih.gov/36374543/ DOI: https://doi.org/10.17219/acem/154858
26. Berbets A, Koval H, Barbe A, Albota O, Yuzko O. Melatonin decreases and cytokines increase in women with placental insufficiency. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; 34(3):373-8. https://www.researchgate.net/publication/332673672 DOI: https://doi.org/10.1080/14767058.2019.1608432
27. Gulati A. Vascular endothelium and hypovolemic shock. Current vascular pharmacology. 2016; 14(2):187-95. https://www.researchgate.net/publication/286220614 DOI: https://doi.org/10.2174/1570161114666151202210221
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Najmah M. Meran, Rifka M. Hussein

This work is licensed under a Creative Commons Attribution 4.0 International License.











 Creative Commons Attribution 4.0 International license..
Creative Commons Attribution 4.0 International license..